Scientists are not exactly the most well-known people in the world, and yet there are a few names among them that have established themselves firmly in the public consciousness.
Alexander Fleming is one of those names, inexorably linked with the discovery of penicillin. Even people who have never studied science or medicine in their lives may have still heard the story of how Fleming’s messiness accidentally yielded the first antibiotic in the world. How he left behind in his lab some Petri dishes with bacterial cultures and, when he came back, one of them developed mold which killed the bacteria, and the rest, as they say, is history.
Well, maybe not just yet. As we are about to discover, the real story was a lot longer and more complicated and definitely involved a lot more people. History might have preferred to condense it down to one manageable, bitesize chunk, but today, however, we are looking at the full course meal.

Early Years & Education
Alexander Fleming came from humble beginnings. He was born on August 6, 1881, at Lochfield Farm near the small town of Darvel in Ayrshire, Scotland. He was the seventh of eight children of Hugh Fleming, with the last four coming from his second marriage to Grace Stirling Morton.
Fleming’s father was a farmer. His mother came from a farming family. He grew up on a large, remote 800-acre farm that was a mile away from the nearest house. He and his siblings spent their earliest years roaming through the nearby valleys, streams, and moors, ensuring that the future man of science will always have a fondness and respect for nature.
The family suffered a major setback in 1888 when Hugh Fleming passed away. His eldest son from his first marriage took over the day-to-day operations of the farm. As for Alexander Fleming, or Alec, as the rest of the family called him, he began his education at Louden Moor School, a small place that only had a dozen or so students of different ages who were all taught in the same classroom. From there, he moved on to Darvel School which was a bit more advanced but required young Alec to walk eight miles each day.
It did not take long for other people to recognize Fleming’s academic potential and, at age 11, he was awarded a scholarship to Kilmarnock Academy, a state-funded secondary school and only one of two schools in the whole United Kingdom (the other being the prestigious Eton College) which had educated two Nobel Prize laureates.
Fleming spent two years at this academy but, when he was 13, he got the opportunity to continue his studies in London. One of his older brothers, Tom, had moved to the city to study medicine and later opened a practice there. Soon enough, four of his younger siblings, Alec included, joined him and lived together in London.
Fleming enrolled in the Royal Polytechnic Institution where, again, he impressed with his book-learning and acumen. He was skipped ahead two years and finished school when he was just 16. From there, he needed a job and found work with a shipping office. He spent four years at that place but later recalled that he did not enjoy the experience.
Going to Med School

In 1900, Alec found a much-needed break from the work he disliked by joining two of his brothers in the Second Boer War in South Africa. All were part of a Volunteer infantry unit called the London Scottish Regiment. However, they never actually saw any action before the war ended and mostly spent their time honing their shooting and swimming skills.
By the time he returned to London, a stroke of good luck befell Fleming. In 1901, when he was 20 years old, he received an inheritance of roughly 250 pounds from his uncle, John Fleming. It wasn’t a vast fortune or anything, but it was enough for him to quit his 9-to-5 job and continue his studies. At the encouragement of his older brother Tom who now had a thriving medical practice, Fleming enrolled in med school.
There is a myth that is still popular today which states that Fleming’s education was paid for by the Churchill family because Fleming’s father once saved Winston Churchill from drowning as a boy. In gratitude, Winston’s father, Lord Randolph Churchill, promised to give young Alexander the same kind of education that his own son would receive. The story continued decades later, during World War II, when Churchill fell gravely ill due to pneumonia, but his life was saved, once again, by Fleming thanks to the penicillin developed by Alexander.
This is quite a fanciful tale and it most likely still persists today because it involves two popular, larger-than-life figures of their time. Unfortunately, there is no evidence to back it up and Fleming himself dismissed it as nothing but a “wondrous fable.” There is nothing on the Churchill side to lend it credence, either, and, as you might suspect, the life of the prime minister has been extensively documented.
Image: St. Mary’s Hospital London
The simple truth is that Fleming obtained an inheritance and, because he had excellent scores in his examinations, he could, more or less, have his pick of colleges. He chose St. Mary’s Hospital Medical School in Paddington because it was close to his home and because he once played water polo against their team. In 1906, he graduated from the school with distinction and began his career in medical research.
This was not his original choice and, in fact, he made it through a strange set of circumstances. At first, Fleming intended to become a surgeon. As it happened, due to his time in the Boer War, Alec was quite a skilled marksman and one of the top shooters on St. Mary’s rifle club team. He was so valued, in fact, that the club captain did not want him to leave which is what would have happened if Fleming became a surgeon. Instead, he convinced the Scotsman to pursue a career in research at St. Mary’s and even got him a position working under Sir Almroth Wright. That way everybody was happy – the rifle club kept one of its top sharpshooters while Fleming got to study under one of the world’s leading immunologists.
Early Research
Here, Fleming was exposed to Wright’s ideas on vaccine therapies which have, undoubtedly, influenced his entire career. In 1908 he graduated with a Bachelor of Science degree in Bacteriology and became a lecturer at St. Mary’s.
CREDIT: Eduard Blum – https://wellcomeimages.org/indexplus/image/M0013322.html, CC BY 4.0
A few years later, Fleming developed a reputation as the go-to guy in London if you were rich and had syphilis. He began administering Salvarsan, a new drug which is known today as arsphenamine. It was created in the lab of German physician and Nobel Prize laureate Paul Ehrlich and, back then, it was the first effective treatment against syphilis. Fleming was introduced to the drug by Wright and amassed a tidy sum of money by being one of the main proponents of Salvarsan in England.
Fleming’s practice and his research progressed along smoothly until World War I broke out. He enlisted and served with the Royal Army Medical Corps as a captain. During his time there, he continued his research into bacteriology in a makeshift laboratory in Boulogne, France. He saw many soldiers die due to infected wounds and couldn’t help but notice that the antiseptics they were using tended to make the injuries worse.
He studied this problem and wrote an article that was subsequently published in the medical journal The Lancet in 1917. Fleming argued that chemicals such as carbolic acid which were used as antiseptics were only efficient in certain cases such as treating surface cuts. When dealing with deeper wounds, the chemicals did more harm than good as they killed the body’s own immunity agents such as leukocytes, and minimized its ability to protect itself from infections. According to his observations, anaerobic bacteria thrived in deep wounds despite the presence of antiseptics.
Fleming opined that, in such cases, it was best to simply keep the wound clean and dry and let nature take its course. His beliefs were echoed by his mentor, Sir Almroth Wright, who also argued that deep wounds should only be cleaned using a simple saline solution but, unfortunately, their recommendations were mostly ignored by field doctors for the rest of the war.
The Discovery of Lysozyme
Even though Fleming is renowned for his discovery of penicillin, he actually made a different breakthrough earlier in his career. This one, however, did not end up having a huge impact on medicine so it tends to get left behind.
After he returned home from the war, Fleming continued his studies into substances with microbial properties and made an interesting discovery while researching nasal mucus. The exact circumstances are somewhat murky as different versions of the story were repeated. Some say he obtained the mucus sample from a patient with a heavy cold. Others say that Fleming himself was working with a cold and had a “Eureka!” moment and decided to investigate his own nasal drippings. And some say that he simply got lucky and a bit of his snot dripped down onto a Petri dish while he was in the lab.
Regardless of how it got there, Fleming wanted to see what effect the mucus would have on bacteria. He mixed the two together and let them sit for a few weeks. When he came back to investigate, Fleming discovered that the nasal substance completely killed the bacterial colonies.
Fleming realized that the secretion must have contained an antimicrobial component that was part of the human body’s innate immune system. It was an enzyme that Fleming isolated and named lysozyme. As he kept researching this new substance, he found that it was present in many other bodily secretions, including tears, saliva, skin, and hair.
Subsequently, the bacteriologist discovered that lysozyme was also present in egg whites which meant that huge quantities could be isolated with relative ease. This could have been a major boon for the field of immunology but, unfortunately, the enzyme was mostly effective against harmless, airborne bacteria rather than anything dangerous. Today, it is mostly used as a food and wine preservative. Even so, it showed Fleming the potential in this kind of research and set him on track to make a discovery that will revolutionize medicine forever.
Penicillin – A Fortuitous Accident
Fleming once wrote: “When I woke up just after dawn on September 28, 1928, I certainly didn’t plan to revolutionize all medicine by discovering the world’s first antibiotic, or bacteria killer. But I suppose that was exactly what I did.”
The scientist was looking for a better alternative to lysozyme. The latter showed itself worthy as a proof of concept, but surely there had to be another substance out there somewhere which was more efficient against dangerous bacteria. To that end, Fleming had begun experimenting and studying the properties of a bacterium called staphylococcus, a nasty piece of work that could cause abscesses, sore throats, and boils.
Fortunately for Fleming (and the rest of the world), the bacteriologist was not exactly a tidy man. In August 1928, he went on a family vacation with his first wife, a nurse named Sarah McElroy, and their only child, his 4-year-old boy named Robert. He grouped up all of his Petri dishes that contained bacterial colonies and left them near an open window in his lab. In some versions of the story, this felicitous carelessness was ascribed to one of his assistants, not to Fleming himself.
When the doctor returned on September 3, he noticed that one dish had been contaminated with mold spores. This annoyed him at first, but then he saw that there were no bacterial colonies near the mold. The latter had killed all the bacteria it came into contact with and inhibited its growth.
Fleming isolated the mold and identified it as a rare strain of Penicillium notatum. He gave his new creation the unfortunate name of “mold juice” and it wasn’t until several months later that he decided that a rebranding might be in order and came up with penicillin.
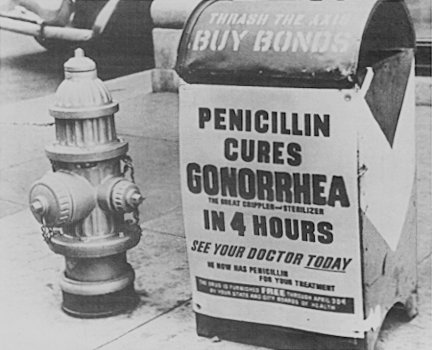
Unappealing name aside, Fleming’s “mold juice” immediately showed great promise as it proved effective not only against staphylococcus, but other harmful bacteria such as meningococcus, streptococcus, and the diphtheria bacillus. The first antibiotic had been created and the world now had a potential cure for pneumonia, gonorrhea, meningitis, scarlet fever, and other infectious diseases.
From Mold to Medicine
Actually, not so fast. In reality, the process of taking penicillin and turning it from a simple mold into a practical medicine was long and difficult and involved a lot of work from many different scientists. Fleming’s role is undeniable, but to give him sole credit for ushering in the era of antibiotics is doing a disservice to many other brilliant minds.
First off, let’s talk a bit about his precursors. Fleming was the first to isolate and identify the bacteria-killing mold and treat other people with it, but the phenomenon itself had been around for millennia. Ancient cultures like the Egyptians were noted for the practice of applying poultices made from moldy bread on wounds to prevent infections. In modern times, an English physician named Sir John Burdon-Sanderson might have been the first to observe and report that certain molds from the Penicillium family could inhibit the growth of bacteria back in 1871. Inspired by his work, Joseph Lister, the father of antiseptic surgery, established a year later that Penicillium glaucum had the potential to kill off bacteria, but never published his findings. Many other scientists came before the Scottish doctor but, for whatever reasons, they were never able to take their own research to a conclusion.
Even Fleming himself found it difficult, at first, to make others care about his discovery. In 1928, he isolated the mold, he called it penicillin and began treating people with it. In June of the following year, Fleming published his findings in The British Journal of Experimental Pathology to a very lukewarm and uninterested reception. Back then, people could not yet see how antibiotics could change the medical world and this included Fleming himself. In the article, he made few mentions regarding penicillin’s potential medical applications and, instead, focused on how it could be used in a mixed culture to separate bacteria sensitive to the mold from bacteria that had no reaction to it.
The main problem was that Fleming discovered early on how difficult it was to work with penicillin. He had two assistants, Stuart Craddock and Frederick Ridley, who were given the arduous task of finding ways to isolate pure penicillin from the fungus which produced it. However, the substance was unstable and they were only able to produce solutions of crude material. For a while, it looked like manufacturing large quantities of penicillin would have been nigh-impossible.
The Long Road to the Nobel Prize
During the 1930s, Fleming continued his research on penicillin but never made that breakthrough that would have turned it into the life-saving drug we know today. The same problems remained all throughout the decade – the penicillin was too impure and could not be mass-produced.
That breakthrough did happen, eventually, but it came from a team at Oxford led by Australian pharmacologist Howard Florey. His group worked in a research department named the Sir William Dunn School of Pathology, better known simply as the Dunn School. They started their work on penicillin in 1939, with the main goal being to isolate and stabilize enough of it to be usable on humans.
Besides Florey, some of the other key members of the Oxford team were German biochemist Ernst Chain, English biologist Norman Heatley and English biochemist Edward Abraham. However, their program needed so much penicillium mold filtrate for animal experiments and clinical trials that, soon enough, pretty much the entire Dunn School worked on the project so we could never fully give credit to everyone who played a part in developing the life-saving antibiotic. Their efforts were also slowed down by another “minor issue” called World War II so it wasn’t like they had an abundance of manpower and resources. In fact, to save on space and materials, they began growing bacteria cultures in whatever vessels they had on hand such as bathtubs, food tins, and even bedpans.
Edward Abraham correctly deduced the structure of penicillin, at roughly the same time as American chemist Robert Burns Woodward. Norman Heatley suggested that larger volumes of penicillin could be produced by extracting it into amyl acetate and then back into water. Chain and Florey discovered how to isolate and concentrate the germ-killing agent found in penicillin.
In 1940, the team used penicillin to protect mice from streptococcus. A year later, a policeman named Albert Alexander became the first human to receive the Oxford penicillin in order to treat a bad infection he had inside his mouth. Although Alexander made a quick recovery in just a few days, they didn’t have enough of the drug to deal with the infection completely and it returned in a few days and killed him. Not an auspicious start, but subsequent patients fared better and showed the world the value of penicillin as medicine.
The challenge of scaling up production of the drug to industrial quantities was eventually taken up by British and American pharmaceutical companies, particularly the Northern Regional Research Laboratory (NRRL) in Peoria, Illinois, a subsidiary of the United States Department of Agriculture.
As you can see, there were many individuals and institutions that played a vital role in the development of penicillin as an antibiotic. For their work, they were awarded the Nobel Prize in Physiology or Medicine in 1945, although it only recognized Alexander Fleming, Howard Florey, and Ernst Chain due to one of the foundation’s most controversial rules of awarding a Nobel Prize to a maximum of three people.
Later Years
Fleming spent his entire professional career as a researcher at St. Mary’s and, in 1946, succeeded his mentor Almroth Wright as head of the hospital’s Inoculation Department which was renamed to the Wright-Fleming Institute. He also served as President of the Society for General Microbiology, rector of Edinburgh University, a member of the Pontifical Academy of Science, and even as Honorary Chief Doy-gei-tau of the Native American Kiowa tribe. In addition to these, Fleming also received pretty much every honorary medal and doctorate and award and all other scientific honors under the sun.
For his part, Fleming always made sure to acknowledge the efforts of Florey and his team in making penicillin a worldwide commodity, but the general public and the media seemed determined to lavish their praise solely on the Scottish microbiologist, probably because the story of his “happy accident” was more enjoyable.
In his later years, Fleming concentrated his efforts on warning people about a problem that we face right now – resistance to antibiotics. Both he and Almroth Wright realized early on that microbes could very easily become resistant to penicillin if the wrong doses were used or for too short a period, with each subsequent generation of microorganisms being more resistant than the last. He wrote several papers on the matter and even mentioned it during his speech for the Nobel Prize.
In his private life, Fleming was quiet and unassuming. His son Robert followed in his father’s footsteps, studied medicine and became a general practitioner. His first wife, Sarah, passed away in 1949 and, unsurprisingly, this had a profound effect on Fleming who buried himself in his work and spent a lot of time alone, in his laboratory, until the late hours of the night.
Fleming’s life brightened up considerably when he met Dr. Amalia Koutsouri-Vourekas who came to work at St. Mary’s. The two fell in love and married in 1953, but their happiness was short-lived. Alexander Fleming died suddenly two years later, on March 11, 1955, of coronary thrombosis. He had been feeling poorly over the last few weeks but was convinced that it was only gastric distress. When he started feeling nauseous on the day of his death, his wife wanted to call a doctor, but he insisted that it wasn’t necessary. He had a heart attack minutes later and was subsequently buried at St Paul’s Cathedral. Alexander Fleming’s life may have been extinguished in moments, but he left behind a life-saving legacy that will live on forever, one that few people in history could ever hope to match.



